The government must commit to its own agenda
A lack of drive and serious commitment to engaging the public is threatening to undermine STPs before they’ve really got started, warns one programme manager.

Bringing together health and social care is crucial to sorting out the problems in the NHS, and could unlock all sorts of benefits for patients. But to make these reforms successful, the government needs to provide more clarity about how they’re going to work – then to demonstrate commitment to its own strategy.
I work in programme management for a Commissioning Support Unit: we support CCGs and other organisations on matters such as finance, IT, service transformation and change management. Recently I’ve been supporting our local system to develop a Sustainability and Transformation Plan (STP) – which bring NHS bodies together with councils and community providers to produce a five-year strategic plan to improve care and find the very ambitious savings required of us.
The benefits of STPs could be huge. The whole system is short of money, and we have a growing and ageing population with increasingly complex needs: to have any chance of sorting this out, we must integrate health and social care services – and STPs have sparked some real collaboration. We’re bringing together people who’ve been plugging away at different aspects of the same problem for years, and there’s huge enthusiasm.
We had a difficult start, though, because NHS England made up the policy on the hoof. Late last year, work had started across England on Local Digital Roadmaps: by April, we were required to submit plans to transform and connect the IT of NHS and social care bodies within our geographical ‘footprint’. Then at Christmas, we were suddenly asked to produce an STP by June.
It wasn’t clear how STPs were to line up with Local Digital Roadmaps, and in some areas their footprints aren’t coterminous – which is daft. NHS England’s guidance was fragmented, emerging in bursts while we worked, often leaving us little time to respond to new requests. Still, we hit the deadline, expecting a written response in July; but as of late August, we haven’t heard back. NHS England are constantly telling us to work “at pace and at scale”. It would be helpful if they worked at the pace that they expect of us!
A second big challenge with STPs is their lack of a formal structure or leadership. ‘Volunteer’ chief executives lead STPs alongside their day-jobs, and the organisations involved report to their own boards – which have a legal responsibility to protect their own bottom lines. So plans that are good for the whole system can lead to individual organisations losing income, which may put boards in conflict with STP ambitions. I think the government should create formal structures that will enable STPs to appoint full-time leaders, make the necessary strategic decisions and, crucially, move money around the system to where it’s needed.
System-wide reforms may also involve controversial changes such as closing A&E departments. Sensibly, NHS England requires strong public and patient engagement before these decisions are finalised: when we don’t get people’s buy-in, the result is protests, judicial reviews – and delays that we can’t afford. So we need to start consulting on our plans and having an open conversation with the public. But NHS England says we can’t publish our STPs – presumably because it’s worried about negative headlines. I think we have a duty of candour here, and NHS England says we must move “at pace”; yet we’re barred from explaining our plans. That’s a problem.
The Sharp End is your chance to tell politicians and civil servants how their policies affect your work and your organisation. A version of this story was also published in the Guardian. To work with a reporter on your own story, email editor@healthcare-manager.co.uk. When requested, anonymity is guaranteed.
Related News
-
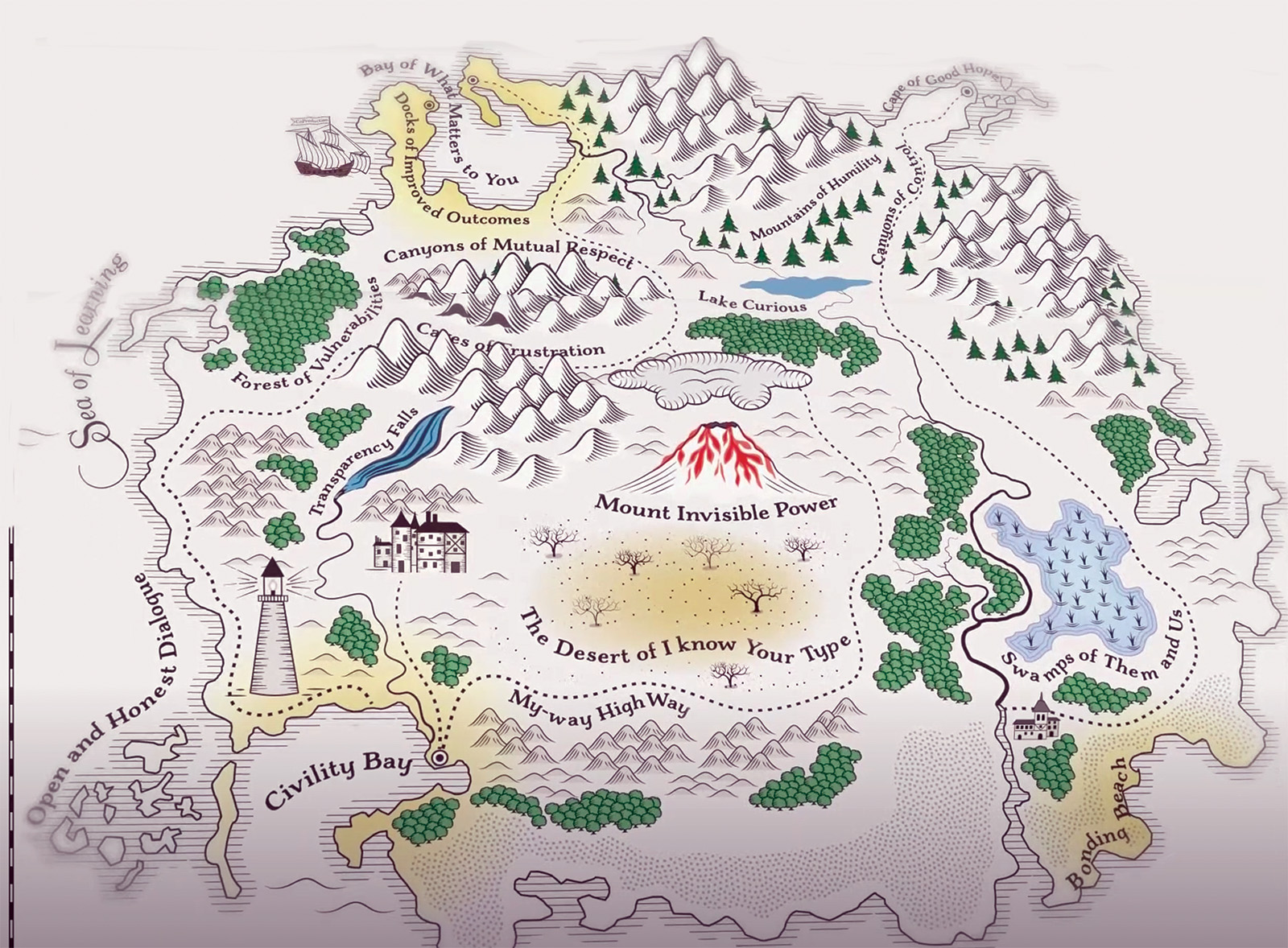
Co-production: say it like you mean it
The NHS talks a good game on co-production, but many patients and carers still feel service changes are done ‘to’ them not ‘with’ them. As Jessica Bradley discovers, meaningful co-production means building lasting relationships and sharing decision making power.
-

Holyrood elections: Back from the brink—for more of the same?
After a big scare last year, the SNP are now clear favourites to extend their rule at Holyrood into a third decade, pointing to incremental reform rather than radical change for the NHS in Scotland. Rhys McKenzie reports.
-

Senedd elections: Tough choices, empty promises
As we enter 2026, the NHS in Wales faces some stark choices and a likely change of government. But the parties vying for power at Cardiff Bay will need to up their game to meet the challenges ahead. Craig Ryan reports.