It’s time to rethink how we do outsourcing
The Carillion collapse shows the perils of driving suppliers to the brink, one support services manager argues. We need to build better long-term relationships to get the most out of our outsourced services.
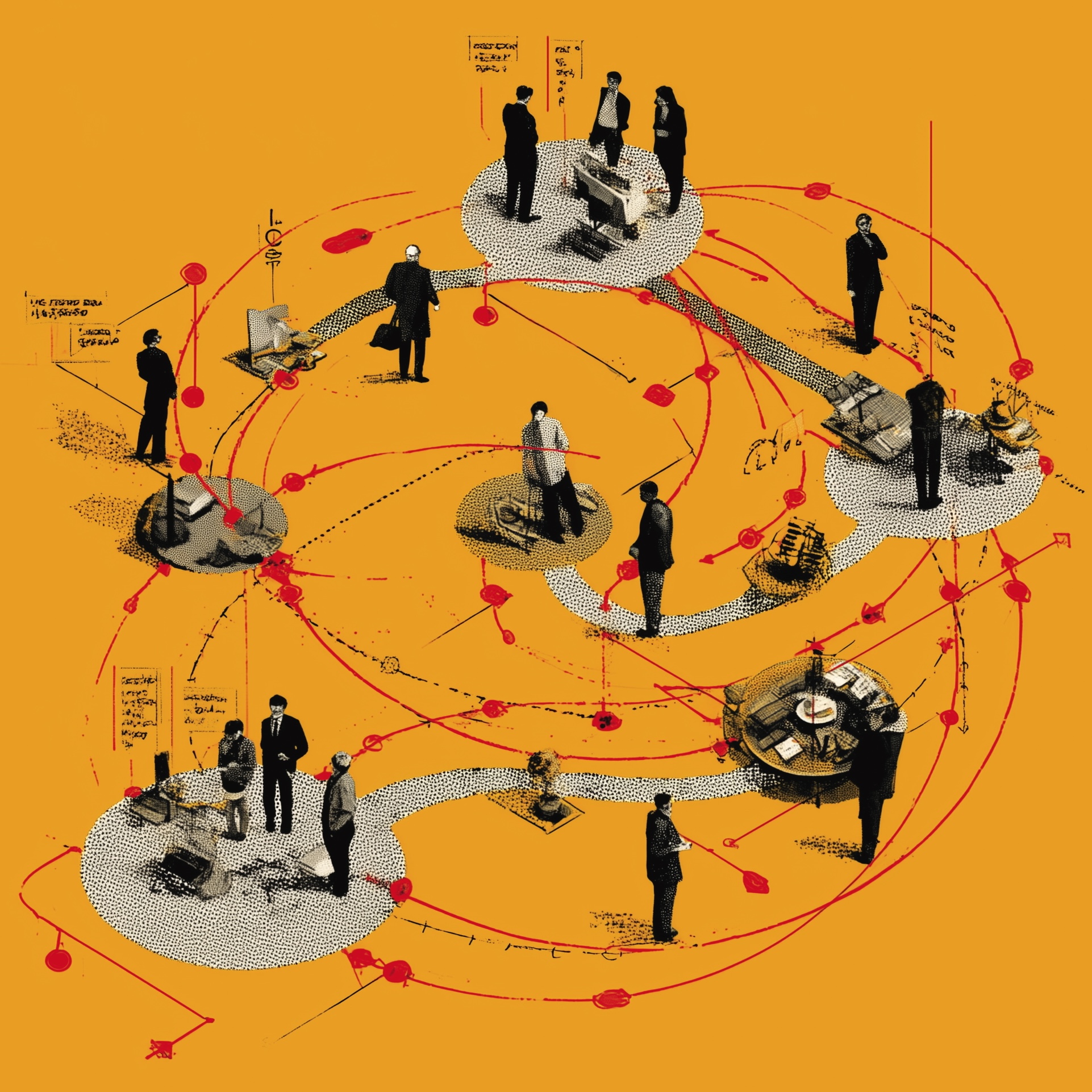
 Illustration: John Levers
Illustration: John Levers

I’m the general manager for an outsourced ‘soft services’ operation in a large hospital, providing services including portering, cleaning and catering.
We’re an outsourcing company – but don’t confuse us with PFI. In PFI hospitals, providers own the ‘hard services’ – buildings and equipment – and their interests can differ sharply from the hospital’s; in that sector, I’ve seen examples of profiteering. But in outsourcing, it’s in everybody’s interests to run things as efficiently as possible – then we and the trust can share the savings.
My staff and I feel that we’re part of the NHS’s frontline services. When there’s a major incident – such as a serious road traffic accident – we work extra shifts without getting client approval for the spending; we rarely get that money back. And we can end up plugging gaps in services: for example, the trust won’t fund meals for people who’ve been waiting in A&E for more than four hours – but we feed them anyway.
In general, though, we run on a very slender profit margin, and we can only do work set out in the contract – under which we’re measured on outcomes, such as the wards’ cleanliness and how quickly we move patients around the hospital.
Saving money
We often spot ways to save money whilst delivering those outcomes. For example, we could deploy fewer porters in departments and more in the central pool. Porters would then spend less time waiting around when their department is quiet, and we could return the money saved to the trust’s estates and facilities department. But the departments like to have their own porters, and the client isn’t willing to persuade departmental staff to get behind changes.
The client also runs separate metrics, measuring work done rather than outcomes – like how long we spend cleaning, rather than how clean the wards are. This deters us from investing in efficiency, because if we achieve the same result more quickly we get a worse score on these metrics; so does the client’s reluctance to share the proceeds of efficiency reforms. If they were willing to focus on outcomes, to share the rewards of efficiency reforms and to push departmental staff to accept changes, then we could save a lot more money for the trust.
We’re already pretty efficient, though. Personally, I’m quite left-wing; but having worked for in-house operations, PFI providers and outsourced services, I’ve concluded that outsourcing can work well for soft services. We can make decisions quickly; we’re held to account against performance targets; we can call on our company’s expertise and systems; and we’re good at working with other businesses involved with the hospital.
We also work closely with health unions, and recognise them as key partners. Union representation ensures that we keep our staff in mind when restructuring services. And as long as we are clear and open with the unions, we find that they and their members work with us to support change in the business.
People worry about outsourcing staff to organisations like ours. But in reality, much NHS labour is already outsourced – simply because trusts are so dependent on locums. Agency people get paid much more than permanent staff, they don’t have to take on as much responsibility, and they can move hospitals when they like. As a result, many people prefer temporary jobs; and that leaves big gaps in trust staffing, creating competition between hospitals that drives locum rates higher still. These people are paid five times as much as my staff – and until the government addresses this problem, it will struggle to contain NHS costs.
Squeezing providers
Meanwhile, trusts are trying to save money by squeezing outsourcing providers – and given our tight profit margins and the risks involved, contracts can quickly become uneconomic. As things stand, providers don’t expect to turn a profit for two years; and it only takes a few things to go wrong to push us into the red. We see the results in businesses like Carillion, where the public sector gets such a ‘good deal’ that the provider collapses and trusts have to pick up the pieces.
An endless focus on price serves nobody. If providers can’t survive on the basic contract, they have to charge for additional labour or services – which encourages sharp practices. And if we’re to meet patients’ needs and invest in efficiency, we need to have a grown-up conversation with trusts: one that emphasises quality as well as cost, and recognises the need to reform operations.
We see ourselves as part of the NHS, working for patients alongside NHS colleagues. But we can only make outsourcing work well if trusts – and the government – are ready to recognise the true costs of delivering services.
The Sharp End is your chance to tell politicians and civil servants how their policies affect your work and your organisation. Most stories are also published in the Guardian. To work with a reporter on your own story, emailthesharpend@healthcare-manager.co.uk. When requested, anonymity is guaranteed.
Related News
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
-
What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.