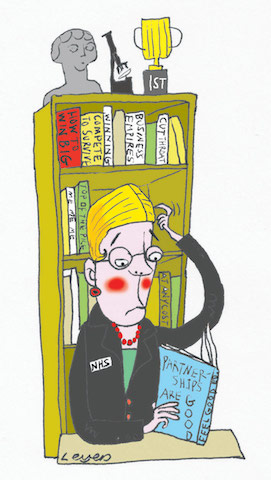
We’re setting leaders up to fail
The needs of the health service have changed dramatically in recent years but, says one NHS leadership coach, many leaders are stuck in an empire-building mindset. They must junk their instinct to compete – and learn to collaborate.
It’s my job to support and develop senior NHS managers. And I’m deeply worried that we’re setting them up to fail – then recruiting more in the same mould.
I’m a former primary care trust director, now working as an executive coach. Many of my clients come from trusts whose leadership has been deemed ‘inadequate’ or ‘requires improvement’ by the Care Quality Commission – but few are genuinely bad leaders. The problem is that they were hired to do one job, and are now required to do something quite different. Yet they’re not being helped to change their approach and, when their trusts run into trouble, they’re being replaced with people likely to encounter exactly the same problems.
Most of these leaders were hired when NHS trusts were being encouraged to compete with other trusts for business, invest in new services and develop their own organisations at the expense of others. To make use of the freedoms granted foundation trusts – including the ability to borrow money at commercial rates – they hired leaders with commercial and financial skills: hard-edged, competitive businesspeople who could expand their ‘market share’.
Re-focusing on collaboration
Then the environment changed. Trusts were – quite rightly – put under greater pressure to improve service quality and patient safety. And demand rose much more quickly than budgets, so the ‘tariffs’ for trust services were cut year after year. Soon, many new services were struggling to repay the investments made in them. In this world, skills in business growth suddenly looked out of place.
Meanwhile, system leaders began pushing a new agenda – one built around collaboration. To protect healthcare we need people to work together, rather than compete, with the emphasis on meeting patients’ needs, rather than the providers’. So both Sustainability and Transformation Plans and the Five Year Forward View create a need for leaders who have emotional intelligence, who are approachable and listen to their staff, who put the public’s needs above the trust’s and who can share power and responsibilities with other organisations.
Let down by the system
So we end up with chief executives being criticised and pushed out – with huge damage to their careers and reputations. But it’s the system that’s let them down: nobody’s given them the right advice or development, and the characteristics once seen as assets have become liabilities.
Unfortunately, trusts’ recruitment practices haven’t changed to reflect this. When these commercially-driven managers fail, trusts are too often replacing them with new figures cut from the same cloth. Job descriptions focus on financial and operational experience, and recruiters are often cynical about the ‘softer’ skills required for staff engagement and partnership working. So trusts select new managers well-suited to facing the challenges of five years ago, and head off towards a fresh set of failures.
Refreshing our approach
What’s to be done? For a start, trusts need to refresh their recruitment practices, taking their cue from NHS Improvement’s new leadership framework, and shift from a narrow focus on technical competences towards a values-based approach. But the NHS cannot afford to lose a swathe of senior managers, and with the right support many of these people could develop the skills we need. After all, we require doctors and nurses to refresh their skills regularly and, these days, the disciplines of management and leadership are changing just as fast as medicine.
The Sharp End is your chance to tell politicians and civil servants how their policies affect your work and your organisation. A version of this story was also published in the Guardian. To work with a reporter on your own story, email editor@healthcare-manager.co.uk. When requested, anonymity is guaranteed.
Related News
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
-

What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.