GP Federations: Empower the professionals who make people healthier
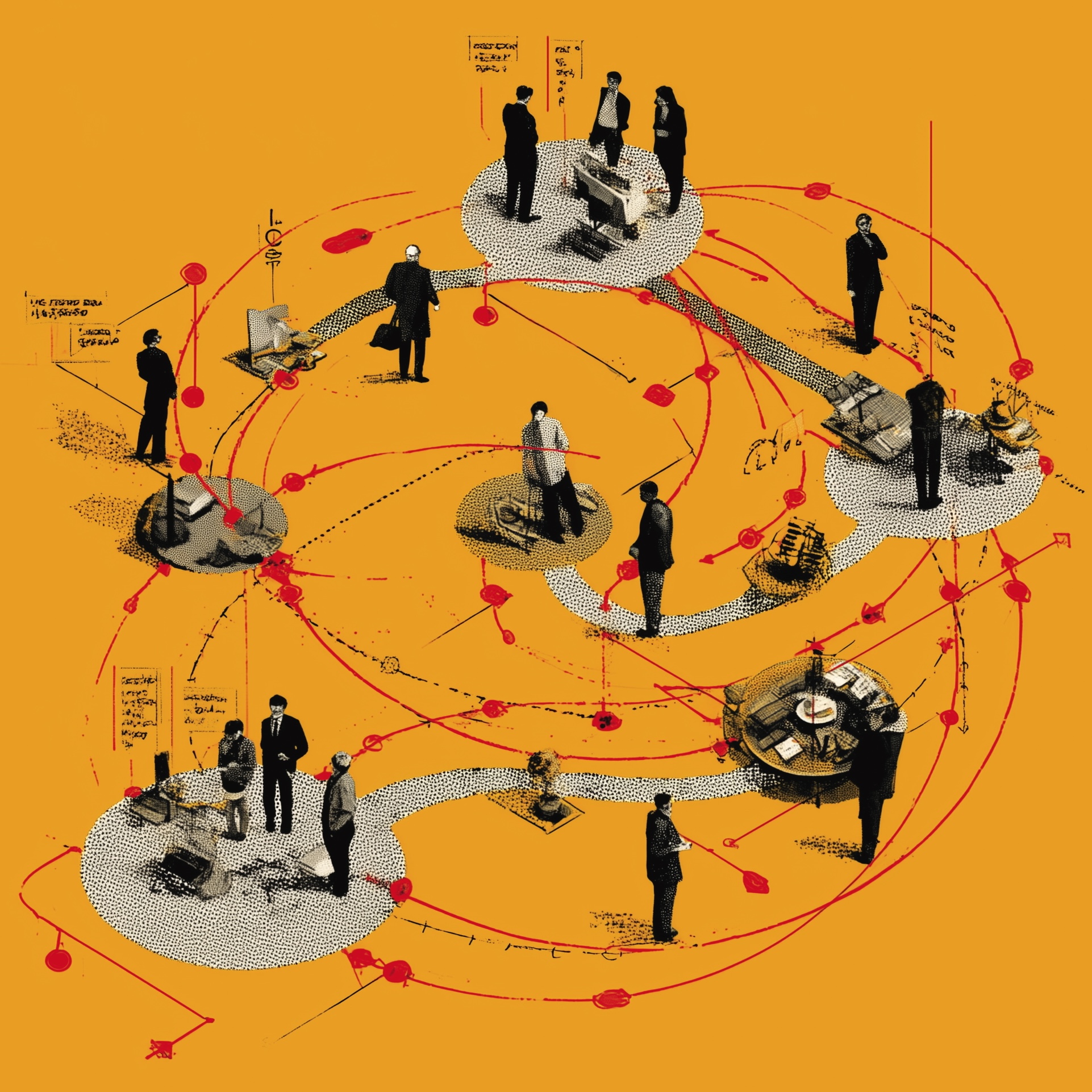
GPs and local councils working together to improve public health is the best way to make the NHS financially sustainable, argues one GP federation manager.

Andrew Lansley’s health service reforms were supposed to put GPs in charge of commissioning health services via Clinical Commissioning Groups (CCGs). And GPs do have the right goals: they want to improve the population’s health. But in reality, they’re often sidelined within CCGs; in the NHS, all the real power lies with Department of Health and Social Care (DHSC) bodies and NHS trusts. I believe we need new alliances between GP practices and local authorities, with a focus on promoting good health. Health and care staff should focus on local relationships and maximising wellness, rather than on top-down structures and delivering treatments.
I’ve worked on national NHS policy, and seen the system from that perspective. But for some years, I’ve been running GP federations: local, non-statutory bodies, owned and run by GPs. These vary around the country, but the ones I’ve worked for have had a strong emphasis on promoting good health.
Federations can do this because GPs’ financial incentives are aligned with their professional ethics. All doctors want to keep people well; but because GPs are paid per patient rather than per treatment, we have a financial interest in minimising sickness rates. For us, higher sickness rates mean overburdened appointment schedules and exhausted treatment budgets.
The commissioner/provider split means that, beyond the primary care offered by constituent GP practices, CCGs can’t offer services themselves. But GP federations can offer services to CCGs – and because these services are shaped by GPs, they often focus on improving health, tend to be well linked into primary care delivery, and make good use of GPs’ excellent patient records.
You’d think that CCGs would share federations’ interests in improving public health and integrating services with primary care. In my view, though, CCGs weren’t designed to empower GPs, but to shift the blame for NHS cuts from the DHSC to local practitioners. CCGs are run by people appointed by government, and often steamroller decisions through, sidelining GP practices and disenfranchising patient groups.
Many NHS trust staff also have a genuine interest in improving the population’s health. But trusts only get paid if sick people need medical attention. Financial imperatives mean they can be actively hostile to health initiatives, and consequently to the federations that champion them. Some hospital trusts lobby CCGs not to award contracts to federations – for example, by leaning on them to bundle up contracts so they include specialist services that only hospitals can provide.
Federations can find allies among local authorities, though. Unlike NHS bodies, councils are directly accountable to local people. And now they’re charged with promoting public health, they tend to focus on prevention. So where the NHS used to offer smoking cessation services, weight loss courses and support for teenage mums, councils concentrate on discouraging people from smoking, over-eating or getting pregnant at a young age in the first place.
Councils even consider goals such as reducing damp in homes as public health work. Some NHS staff don’t see the relevance, but councils were originally created to tackle these environmental issues: their early work to provide people with clean water, for example, led to a huge improvement in public health. In contrast to many NHS colleagues, I actually think that councils’ public health work has been better targeted and more effective than the NHS’s efforts.
In my ideal world, councils would commission our health services; unlike NHS bodies, they have an interest in reducing demand for medical treatments. That’s not going to happen – but we could make smaller changes that support more efficient and effective health services. We could let GP federations run community nursing, for example; managed within one organisation, GPs and nurses could collaborate much more effectively to support and protect patients in the community.
Meanwhile, GP federations and local authorities should make common cause. Federations can get involved with the scrutiny committees of council-run Health and Wellbeing Boards – councillors and local authority staff are often willing to work with federations to strengthen their public health work.
NHS trusts delivering amazing medical services. But it’s neither financially sensible nor ethically justifiable to carry on delivering ever more medical treatments to an ever more sickly population. We need to empower the professionals who focus on making the public healthier: GPs and local authorities, with GP federations acting as a bridge between them. And given changes to payment systems, hospitals could also play their part.
Working together, we need to understand and address the key determinants of ill health; for it’s only by fostering a healthier population that we’ll create a sustainable, effective NHS.
The Sharp End is your chance to tell politicians and civil servants how their policies affect you. To work with a reporter on your own story, email thesharpend@healthcare-manager.co.uk using a personal email address. When requested, anonymity is guaranteed.
Related News
-
What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.
-

We get knocked down. We get up again.
With its brutal NHS cuts and chaotic reform plans, the government is moving fast and breaking things (again). It will be up to managers to fix them (again), writes Geoff Underwood.