The confused centre is holding us back
Dean Royles, director of HR and organisational development at Leeds Teaching Hospitals, calls for a more streamlined system to run the NHS in England.
We in the NHS are constantly trying to deliver better services with flatlining resources. In previous years, I have lobbied for better funding, but we know that we could also work more efficiently and effectively.

The frontline NHS workforce is dedicated to improving patient services and reducing waste. There are many good examples of major efficiency savings and new ways of working which have begun to scratch the surface of this funding gap.
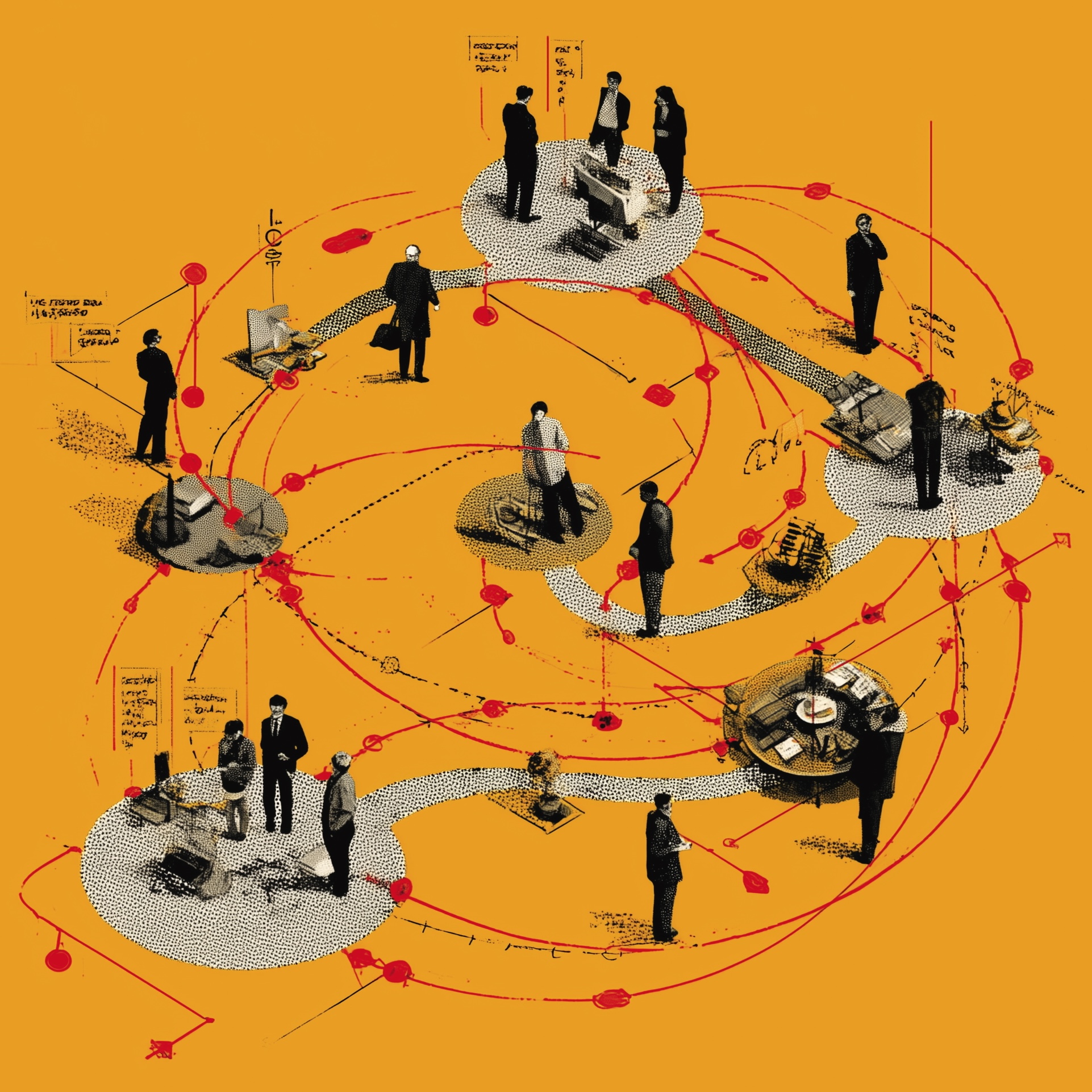
Unfortunately, our efforts to make fundamental and lasting improvements are being hampered by a very confused organisational landscape at national level in England, where six statutory bodies are sending out conflicting messages and competing over policy territory. They can seem more focused on defining and protecting their roles than on supporting health providers to deliver good services.
Overlapping responsibilities
I’ve spent 30 years in NHS HR, working for many different trusts and national bodies, and throughout my career there’s been tension around how the centre relates to providers. It’s nothing new, but the problem feels particularly stark today.
There’s little clarity in the division of responsibilities between the Department of Health, NHS Improvement, the Care Quality Commission, NHS England, Public Health England and Health Education England. The result is a lack of coherent strategic management across our health services, which affects how we do our jobs and the cost-effectiveness of the NHS – and could damage patient services.
One example is the ending of bursaries for student nurses. We’ve seen lots of media coverage of the extra costs of qualifying as a nurse. The centre defended the decision but missed the opportunity for a national campaign to boost nurse recruitment, and I’m sure that’s partly because it’s not clear who’s doing what. I believe a campaign similar to those for recruiting teachers would have helped avoid the fall in student nurse applications we’ve seen.
Turf wars
We see the same problem with national bodies publishing conflicting guidance, or getting involved in policy fields outside their core roles. In theory, the DH has largely passed provider guidance work to NHS Improvement – but it still puts out lots of material. NHS Improvement publishes guidance on consultant job planning, which you’d expect to come from NHS Employers. And of course everyone has a view on the implications of Brexit.
When the Getting It Right First Time team (GIRFT), which identifies variations in hospital care, recently argued for more consistency in commissioning, NHS England responded that GIRFT has nothing to do with commissioning and that CCGs must be free to make decisions locally.
Many believe the underlying problem is that Andrew Lansley’s reforms have never operated as intended; these statutory bodies were created for a system that doesn’t exist. Lansley wanted to put clinicians in the driving seat as commissioners, believing that patient choice and competition would improve quality. But it seems to me that CQC inspections have become the main drivers of quality. Meanwhile, the DH, which was supposed to leave hands-on management to NHS England, hasn’t in fact relinquished its traditional roles. The result is that national bodies appear introspective and key policies lack a single, clear voice.
Aligning incentives
Sustainability and Transformation Plans are exposing these weaknesses. STPs require delivery bodies to compromise some individual goals for the greater good. However, regulators like NHS Improvement and the CQC still hold each provider to account individually. STPs are essentially voluntary partnerships that managers are asked to pursue around their day jobs, and so we’re often disincentivised from co-operating on common goals such as reducing the use of agency staff.
We need more strategic direction acc oss the system, rather than a complex set of national regulators and performance management systems that don’t line up with current policies. For years we’ve tried to manage the impact, but experience shows we now need another solution.
I understand people’s reluctance to embark on a new wave of NHS reforms. But I think we need fresh legislation to bring much greater clarity to organisations’ responsibilities and rebuild performance management around today’s policy goals.
Providing better care for an ageing population is the aspiration of all my colleagues working on the frontline. To achieve that, we all need to work towards and support the same goals – from the centre out. In my opinion, that demands a new, more streamlined system.
The Sharp End is your chance to tell politicians and civil servants how their policies affect your work and your organisation. To work with a reporter on your own story, email editor@healthcare-manager.co.uk. When requested, anonymity is guaranteed.
Related News
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
-
What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.