Never mind the ‘ology
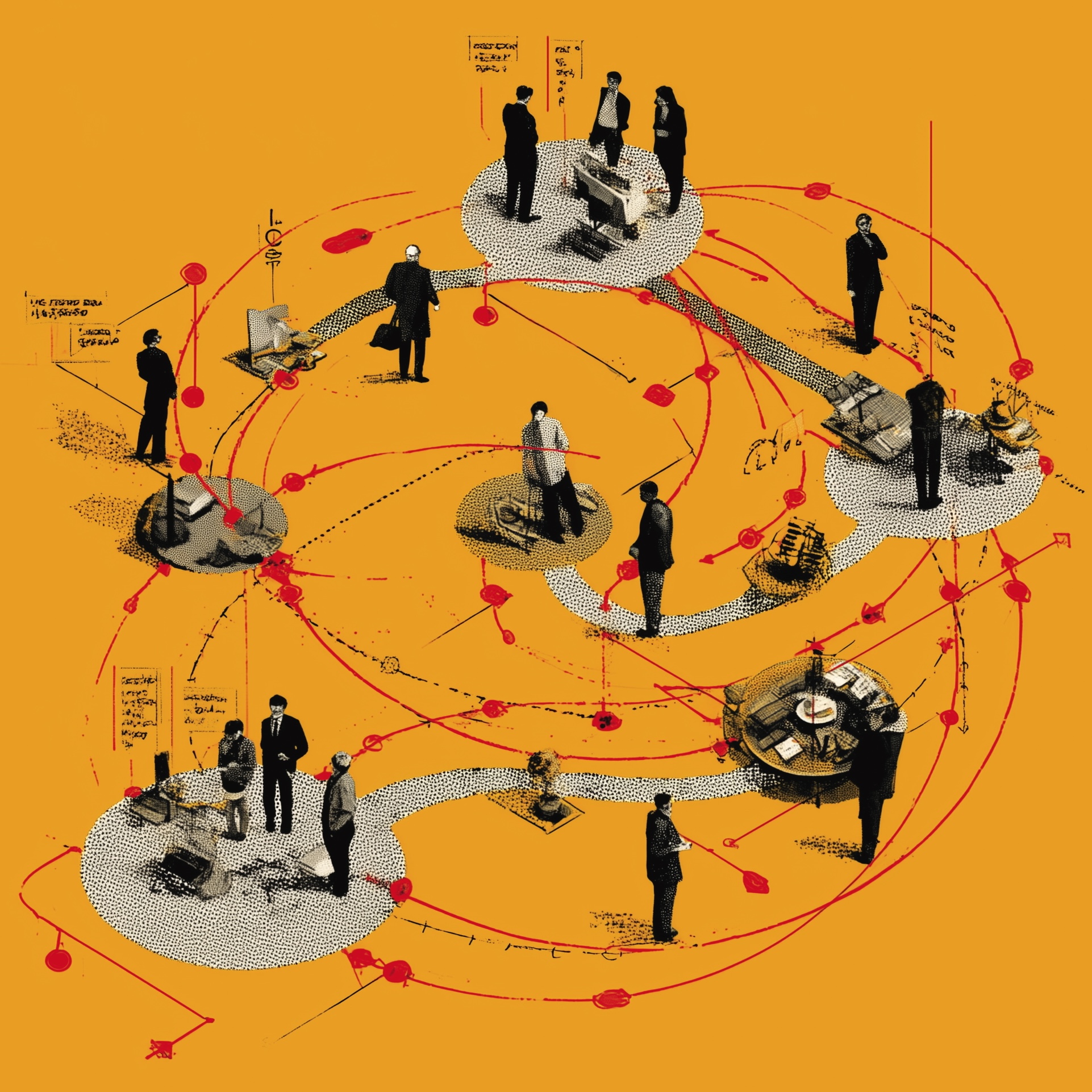
Teams of doctors from different specialisms working shifts together helped the Countess of Chester Hospital to weather the Covid storm with increased patient satisfaction and better staff engagement. Here’s how they did it.

Until spring last year, the Countess of Chester Hospital was working to rhythms familiar to many a medium size district general hospital in England.
“It’s a reasonably normal hospital—with all the usual specialities plus a regional vascular surgery service that we host for three other hospitals,” explains executive medical director Darren Kilroy. “But we were then hit hard with a very abnormal situation.”
Due to “phenomenal” clinical dependency, “the bed base of the hospital was becoming overwhelmed with just one type of patient: medically unwell Covid-19 patients,” he says.
Traditional clinical activity, such as general surgery and elective orthopaedics, was put on hold, and “literally stopped” for many doctors. “We had to think quickly about how we could best deploy this ‘spare’ medical capacity” into something that was actually needed on the ground,” Kilroy adds.
A new operating model
It became clear that the hospital’s operating model would have to change. The trust set up an internal command and control structure with daily Covid-19 operation operational planning meetings to discuss where best to place resources, including staffing. New ideas were put forward, including creating specialist teams responsible for things like ‘proning’—turning patients onto their stomachs to help with breathing.
Kilroy, who has taken a strong interest in medical workforce matters during his career, says, “It became clear that the best thing to do would be to stand down all the normal traditional rosters in the hospital and instead redeploy all our medical juniors and all the medical seniors that we could find onto a shared whole-hospital roster.”
The medical staffing team were asked to identify everyone in the organisation who was available to work, recognising that risk-assessments meant some were unable to provide frontline care.
“We essentially divvied up the available wards and the available doctors, to put small but reliable teams of doctors on each ward around the clock with a full shift pattern,” Kilroy explains. Doctors’ readiness to deliver what Covid patients needed became more relevant than their individual specialties. “We allocated doctors to different ward areas, not based on their ‘ology, but based on their availability to provide care,” says Kilroy.
Managing clinical risk
 Darren Kilroy: “With some of the juniors way out of their depth clinically, it was a calculated risk – it was either that or doing nothing, as we just couldn’t find enough doctors to cope with the demand.”
Darren Kilroy: “With some of the juniors way out of their depth clinically, it was a calculated risk – it was either that or doing nothing, as we just couldn’t find enough doctors to cope with the demand.”
It was important it was to address key safety issues and engage clearly and “honestly” with staff over the roster changes, Kilroy says, because “we were undoubtedly exposing these doctors to a clinical risk they wouldn’t otherwise have run.”
This meant ensuring adequate rest breaks for those staff engaged in intensive and potentially distressing clinical work, and careful planning to ensure there were sufficient supplies of personal protective equipment (PPE), especially for staff working in ‘hot’ areas with very infectious Covid patients.
“We had to make sure that wherever we put the junior doctors we were giving them the best possible PPE and personal protection. We were sort of risk-stratifying which staff went where on that basis.”
“We briefed everyone in some detail around the rationale for what we were doing, rooting it in safe patient care,” says Kilroy. “We spoke very frankly to the juniors, through the educational team and their clinical leads.”
It meant supporting doctors being asked “relatively basic but essential” clinical tasks, such as taking observations or prescribing fluids and drugs, that they may not have undertaken since the beginning of their NHS careers. Some surgeons, for example, had not had to care a medically poorly patient for many years.
Kilroy says, “We accepted that some of these doctors would feel uncomfortable in those settings, so we provided mentorship or buddying for those who felt they were exposed clinically.”
With some of the juniors arguably “way out of their comfort zone clinically”, Kilroy admits there was a risk of clinical harm. “It was a calculated risk, because it was either that or doing nothing, as we just couldn’t find enough medical doctors to cope with the demand.”
Reliable and consistent
The changes made provided each ward with greater and more reliable medical resources, says Kilroy. Nursing staff liked the system because they knew consistently which junior doctors which were going to be on their ward each day, and teams valued having a “clear line of sight to a senior doctor” who could provide guidance and support when patients became unwell.
Kilroy says many of the junior doctors “enjoyed being part of a team and mucked in with the eye doctors, ENT and dental doctors, getting involved in basic clinical care, rediscovering skills they had lost and teams they hadn’t worked with for ages.
“Everyone in the hospital got together behind this roster. You could see there was cohesion around this contribution to keeping these patient safe in a very visible way. There was an overall uptick in engagement.”
Education and training challenges
While it was clear that reconfiguring working patterns could meet the needs of the moment in terms of delivering at least rudimentary services in an emergency, there were concerns about impact on the education of specialist trainees and whether they would be able to meet medical curriculum requirements.
Kilroy says the trust kept Health Education England regional colleagues informed throughout about what the hospital was doing and gained their support and confidence. There was “recognition in the background” that people’s training programmes might be delayed.
“I think they [HEE] were as satisfied as they could be that we were giving juniors really useful extra clinical knowledge around basic patient care. These were highly transferrable skills for everyone and would be of value to them whatever career they had.”
Quality metrics up, complaints down
The whole-hospital roster was in full effect for about 6 months, before it was stood down, and Kilroy says is has had a positive impact on hospital performance.
“All the metrics relating to quality and safety either stayed intact or went up,” he says. “Patient complaints rocketed down. Sepsis screening, sepsis management, falls with harm, pressure area care—all those things that form part of a standard quality metrics pack—they were all as good as, if not better than you’d expect normally for a trust like ours.”
Kilroy is particularly satisfied that “we managed to get everybody in the medical workforce through safely in one piece.” He likes to think that the rostering system helped to support staff health and wellbeing “but whether that is cause or correlation I’m not sure,” he says.
As Covid numbers began to decline the system was modified into “a sort of mini-version”, where some teams of traditional medical juniors continued to work in Covid-19 “zones” while teams of surgical trainees were “released” back into their home disciplines.
“Obviously we’ve reverted back to normal practice because we’ve got to get on with recovery and restoration of normal clinical work. But we could probably switch the whole thing back in about 48 hours if we needed to,” says Kilroy. “It’s there in the background and it’s really good insurance policy for the next time we have a problem.”
- The country needs to know about the extraordinary work NHS managers have been doing during the Covid-19 emergency. If you or your colleagues have a story, get in touch with the editor and we’ll make sure it gets told.
Related News
-

NHS job cuts: you’ll never walk alone
As the NHS redundancies in England loom, Rhys McKenzie explains how MiP will back you, and how members supporting each other and acting collectively is the best way to navigate this difficult process.
-
What now? Seven expert takes on the Ten-Year Plan
The government’s Ten-Year Plan for the NHS in England has met with enthusiasm and exasperation in equal measure. We asked seven healthcare experts to give us their considered view on one aspect that interests, excites or annoys them.
-

NHS job cuts: what are your options?
When politicians start reforming the NHS, there is only one certainty: some people will lose their jobs. But what options might be on the table and how does redundancy work? Corrado Valle explains.