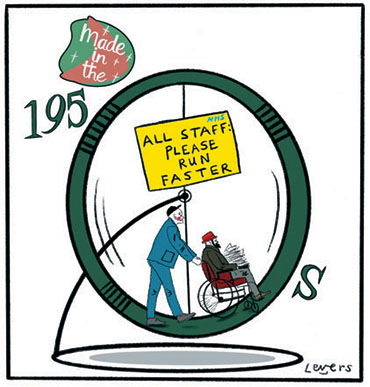
Fundamental change is needed to rescue the NHS from the 1950s
Courageous, system-wide change is the only way to stem increasing demand for medical care and meet the needs of today’s population.
I spent over 25 years in the NHS, ending up as a commissioning chief executive. The NHS’s commitment to meet everyone’s needs free at the point of delivery remains an inspiring purpose. But over the years, Britain’s health challenges have changed beyond recognition, whilst the form of service delivery has barely evolved. If we don’t rebuild the NHS for the 21st century, it will become ever more unaffordable, ineffective and, ultimately, irrelevant.
The NHS is a victim of its own success. Thanks to pharmaceutical advances and acute intervention, today’s elderly people are living 20 years longer than their parents – but many have multiple chronic conditions. They need support in their home, provided by integrated, community-based health and care services; they expect choice and a measure of control; they want to communicate by email and text. Instead, we tell them to get a GP referral, summon them by letter for an outpatients appointment, then put them on a waiting list.
Meanwhile, investment in other services that determine health – such as housing, education and social care – has been cut to the bone. And the resulting problems end up with the NHS: around 30% of hospital in-patients are there simply because we lack the services to support them in the community.
1950s services
Using digital technologies, other sectors have transformed delivery and cut costs by rebuilding the business models – but in the NHS, progress is glacial. Hospitals still routinely do face-to-face follow-ups. We resist providing digital or phone consultations, then complain when businesses meet that demand. We can’t afford to keep delivering 1950s-style services; but rather than changing how we operate, we just keep asking for more money – and we already absorb nearly 20% of all public spending.
The workload is mainly multiple morbidities and mental health problems, but the system is built around acute hospital services, focused on individual parts of the body. We fail to support people in managing their conditions, then intervene in a crisis – keeping them alive, but with increasingly poor quality of life. And everyone runs faster and faster around the hamster wheel, trying to keep up with ever-rising demand.
Why we can’t adapt
Three key factors prevent us from adapting. First, Andrew Lansley’s reforms destroyed system leadership. As locally-focused bodies, built around independent contractors and with limited responsibilities, Clinical Commissioning Groups lack the experience, levers or motivation to rebuild delivery models. And there’s no legal framework to support emerging ‘system lead CEOs’ to fill that vacuum. So nobody has the authority to see through controversial changes; and in the NHS, every change is controversial.
Second, as a workforce we resist change. Managers often blame doctors for blocking systemic reforms, but it’s only human to resist changes that threaten personal influence, status, security and working habits. And senior staff have the status, organisations and resources to produce an awful lot of resistance.
Third, both main political parties are determinedly looking the wrong way. The Tories know that Lansley’s reforms were the wrong intervention at the wrong time, but don’t want to go back there. And Labour is invested in a fantasy of the 1950s NHS; the only things they complain about are underfunding and privatisation. So there’s a lack of political will to address the fundamental challenges.
Disruptive, system-wide change
So what’s needed? System leadership over population-wide health and care, provided by large-scale commissioners able to make unpalatable decisions about system change and investment. And financial flows that favour prevention, community services and care in the home, bridging the gap between health and social care.
That sounds like a mammoth task – but we’ve shown we can deliver disruptive, system-wide changes. In the 1980s we moved 100,000 people out of psychiatric hospitals into the community, shifting funding from the NHS to community provision, social care and benefits. If you point NHS staff in the right direction and give them the right incentives, levers and tools, they’ll do amazing things.
That means changing business models – both system-wide, and within every NHS and care provider in the country. Fragmentation of responsibilities and regulation make that difficult. Yet unless we fundamentally change the way we manage health and care, we’ll remain stuck in this loop – constantly asking for more money to inefficiently deliver ever more technical interventions; extending lifespans, but leaving people’s quality of life dependent on their ability to self-fund social and residential care.
Thirty years ago, we deinstitutionalised people with mental health conditions. It was controversial at the time, but nobody now believes it was the wrong call. Now we need to find the same courage – and deinstitutionalise care of the elderly.
Sophia Christie is a former NHS trust chief executive, and director of strategy and design consultancy UKPrime Ltd. The Sharp End is your chance to tell politicians and civil servants how their policies affect you. To work with a reporter on your own story, email thesharpend@healthcare-manager.co.uk. When requested, anonymity is guaranteed.
Related News
-

The inspector falls: why the CQC needs a fresh start
After years of chaos, the Care Quality Commission urgently needs to rebuild trust and credibility with the public and the services it regulates. What needs to change and what are the priorities for new boss Sir Julian Hartley? Alison Moore reports.
-

Voice, value and vision: what analysts need from the NHS
Data analysts play a vital role in an NHS which is increasingly data-driven and focused on public health trends. But the NHS faces fierce competition for skilled analysts and many feel the health service fails to value them or fully use their talents. Alison Moore reports.
-

It ain’t what you do, it’s the way that you do it
The government’s upcoming ten year plan will try yet again to shift the NHS towards community, digital and prevention. The big question is how, writes Craig Ryan. Try honesty, patience, focusing on what matters and empowering staff and local managers—that’s what gets results.